[ad_1]
This article was previously published December 20, 2020, and has been updated with new information.
“The Immunity Fix: Strengthen Your Immune System, Fight Off Infections, Reverse Chronic Disease and Live a Healthier Life” is a book written by James DiNicolantonio, Pharm.D., with whom Ico-wrote “Super Fuel,” and Siim Land, an esteemed biohacker and author of “Metabolic Autophagy.”
In it, they review how to improve and regulate your immunity — a topic that should be high on anybody’s list these days. The catalyst for this collaboration was a number of academic papers written by DiNicolantonio on the underlying reasons for why some people suffer worse COVID-19 outcomes.
Many who end up with severe illness produce low amounts of Type 1 interferon. There’s also a reduction in their adaptive immune system. As a result, they don’t clear the virus quickly and end up having to rely on a more proinflammatory killing of the virus inside their cells instead.
Immune System Basics
As a refresher, your immune system consists of two primary “arms”:
- The innate immune system, which is your first line defense made up of natural killer (NK) cells, macrophages and white blood cells like neutrophils
- The adaptive immune system — T cells, and B cells that produce antibodies
As explained by DiNicolantonio:
“We used to think that the adaptive immune system was this system that takes a while to kick in, and once you have immunity from your adaptive immune system, then you have a longer-term protection, which is true. However, the adaptive immune system also seems to have cross sensitivity, meaning if you’ve been exposed to previous coronaviruses, your T cells seem to have some cross sensitivity to SARS-COV-2.
So, essentially, what we see is a reduction in T cells, in the cytotoxicity of these CD8 T-killer cells, which kill viruses in a nice, apoptotic, controlled way.
When you have a reduction in those types of immune cells, you have to rely more on your proinflammatory innate immune system for clearing viruses — things like neutrophils, white blood cells, macrophages. They kill in a much more pro-inflammatory, non-specific way, and they end up killing healthy bystander cells.
What we think is going on is, essentially, you have this reduction in Type 1 interferons … which interfere with the virus. And at the same token, you have a reduction in B cells and T cells. So, what ends up happening is you don’t clear the virus as quickly, and you end up having this proinflammatory killing.
Siim and I collaborated because these things are complex. We need to get this in layman’s terms. What our book boils down to is that your diet and your lifestyle control those types of things, and there’s things that you can do to support your own immune system.”
Your T cell function tends to decline with age. It’s also reduced in those with chronic disease. Reduced T cell function appears to be a primary cause of severe COVID-19, seeing how those with the worst COVID-19 outcomes are the elderly and/or those with comorbidities such as diabetes, hypertension, metabolic syndrome and cardiovascular disease.
These factors worsen the proinflammatory response that you get from SARS-CoV-2, but they also weaken your immunity in general. “The Immunity Fix” reviews lifestyle strategies that help you sidestep and prevent this proinflammatory response. “It’s a very holistic approach to looking at the immune system,” Land notes.
Top Two Nutrient Deficiencies to Address
Diet and nutritional supplementation are two key strategies that can help boost your immune function. According to Land and DiNicolantonio, vitamin D may be the most important nutrient in this respect. Vitamin D activates more than 2,000 genes, DiNicolantonio notes, including vitamin K-dependent proteins and repair genes. It also helps your body produce powerful antimicrobial and antiviral peptides.
Those over the age of 60 have a ninefold greater risk of dying from COVID-19 than that of younger individuals. If you’re severely vitamin D deficient, your risk can be 15fold greater. So, while you cannot change your age, you can certainly alter your vitamin D status, thereby potentially minimizing your risk.
However, in order to convert the vitamin D into its active form, you need magnesium, so magnesium would probably be the second-most important nutrient deficiency to address. Magnesium is also required for immune cell function, so if your magnesium level is low, your immune function could be impaired.
“People who have genetically low magnesium in their natural killer (NK) cells and their CD8 T-killer cells … their immune system is down. They have chronic activation of Epstein-Barr, which 95% of us are infected with, and they’re at a much higher risk of lymphoma,” DiNicolantonio says.
“And that’s just one nutrient. Being deficient in one nutrient can potentially cause this immunodeficiency essentially. So, in the book, we go through how nutrients and your immune system interact and why nutrient deficiencies are probably leading to a lot of these poor COVID-19 outcomes.”
Zinc and Selenium Are Also Important
In terms of importance, zinc would probably nab the third spot. Taking zinc lozenges at the first onset of cold symptoms has been shown to cut the duration of the common cold by six to seven days, but you have to take it correctly.
“If you’re using lozenges, you have to take it every two hours,” DiNicolantonio explains. “You got to take it within 24 hours of symptom onset. You have to take about 18 milligrams per dose, and you have to get the total daily dose over 75 milligrams.”
Fourth on the list would be selenium. Not only is selenium deficiency associated with a fivefold higher risk of dying from COVID-19 and a threefold higher risk of having a poor COVID-19 outcome, but it is also associated with coxsackievirus-induced cardiomyopathy (Keshan disease).
So, if you’re deficient in selenium, a nonvirulent RNA virus called coxsackievirus, which typically only causes hand, foot and mouth syndrome in certain children, can become much more virulent, leading to virally induced cardiomyopathy. Patients with this cardiomyopathy, known as Keshan disease, are typically given selenium. Selenium is also important for the production of glutathione, which appears to play a significant role in COVID-19.
The Importance of Melatonin
Another thing that is associated with improved COVID-19 outcomes is melatonin. DiNicolantonio explains:
“Melatonin is interesting. I kind of view it like molecular hydrogen but with some additional advantages. Melatonin can freely pass into any cell membrane, so that’s very key. If you want to get to the oxidative stress, you have to be able to access it and get into the mitochondria. Melatonin and molecular hydrogen are two molecules that can do that and really do that well …
Melatonin is not just this hormone we secrete in the brain. We synthesize it from serotonin, and it can be produced in many cells. So, it’s active throughout the entire day. What’s interesting is that it’s one of the only molecules that seems to increase the transcription of Nrf2.
Most plant polyphenols and all these other Nrf2 boosters only inhibit the inhibitor of Nrf2, which is KEAP1. Essentially, they’re making the current Nrf2 levels more active. When you add melatonin, that increases the transcription of Nrf2. Very few molecules can actually do that.
And Nrf2 is how we boost our endogenous antioxidant enzymes. Really, that’s the key. If you have acute respiratory distress, you want to boost your overall endogenous antioxidant systems, and the best way to do tha is through Nrf2 activators, particularly melatonin.”
High-Dose Melatonin Reduces COVID-19 Mortality
As for dosage, a recent case series involving 10 patients with COVID-19-related pneumonia used 36 to 72 mg of oral melatonin per day in four divided doses, which is far higher than recommended for sleep. DiNicolantonio comments:
“It’s so safe. Doses of melatonin up to 1,000 mg per day in humans have shown virtually no side effects besides grogginess and sleepiness … Melatonin use is associated with an 83% reduction in mortality from COVID-19, a 30 to 50% reduction in testing positive for SARS-COV-2, and in a case series of 10 COVID pneumonia patients, it cut the duration of hospital stay by five days.
And none of those patients who got melatonin ended up on a mechanical ventilator or died whereas in similar severe COVID-19 cases that were hospitalized at the same time, 25% to 40% of those individuals ended up on mechanical ventilators or died.”
As explained by DiNicolantonio, melatonin is actively produced throughout the day and is a master antioxidant, meaning it scavenges free radicals. It also binds to melatonin receptors that upregulate your innate antioxidant defense systems.
“Melatonin actually seems to concentrate in the bone marrow and that’s important because your immune system comes from stem cells produced from your bone marrow,” DiNicolantonio explains.
“From those stem cells, you get your immune cells. Some of your immune cells can even produce melatonin. We think it’s being concentrated in the bone marrow to protect immature stem cells and immune cells from oxidative damage, which actually makes a lot of sense.”
Nebulized Hydrogen Peroxide
While Land and DiNicolantonio hypothesized that inhaled molecular hydrogen at 2% or 3% would be a potential important strategy in COVID-19 patients requiring ventilation in a hospital, this can be significantly expensive. A better alternative, in my opinion, would be nebulized hydrogen peroxide, which you can do at home. This is my personal go-to strategy, and I’ve seen many recover from COVID-19 using this strategy.
You can review my video below for more detailed in formation.
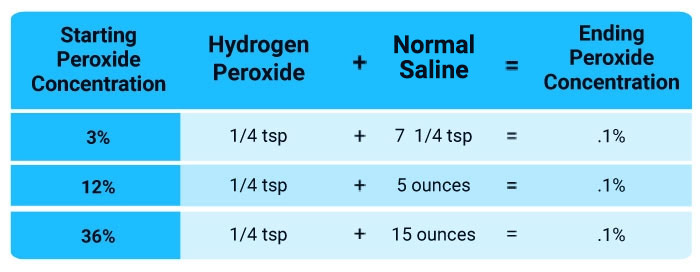
Nebulizing hydrogen peroxide into your sinuses, throat and lungs is a simple, straightforward way to augment your body’s natural expression of hydrogen peroxide to combat infections and can be used to support the immune system.
All you need is a desktop nebulizer, food-grade hydrogen peroxide and some saline. That way, you have everything you need and can begin treatment at home at the first signs of a respiratory infection. Keep in mind food grade hydrogen peroxide must be diluted down to a 0.1% dilution before use.
I believe the hydrogen peroxide works like a signaling molecule, and may even have some direct viricidal effect on the cells in the lining of the lungs and the sinuses where the virus takes hold initially. So, you’re potentially killing it directly, plus supporting your immune responses.
Address Your Metabolic Health
In addition to addressing nutrient deficiencies, in particular vitamin D, magnesium, zinc and selenium, Land stresses the importance of optimizing your metabolic health.
“Research [has found] that metabolic syndrome, obesity and diabetes, all those things, worsen the outcomes of COVID-19 as well as other infections like influenza. Obesity also increases the duration that you can carry the virus and share it for longer. So, it’s especially negative in a society that tends to be in poor metabolic health.
One interesting thing that we discovered during the writing of the book is that one of the molecules that gets activated during an infection is called HMGB1, which stands for High Mobility Box-1.
That gets activated during an infection, and it’s one of the key molecules that kind of offsets the cytokine storm by activating NFKB and NLRP3 inflammasome and eventually causes this massive pro-inflammatory cytokine response …
What we theorized based on this research, is that hyperglycemia, insulin resistance, elevated blood sugar will make it more likely that HMGB1 is going to get into the cell and turn on NFKB and these other pro-inflammatory cytokines that will eventually lead to the cytokine storm.”
The Case for a Low Linoleic Acid Diet
DiNicolantonio and I discussed the importance of avoiding seed oils in our book, “Superfuel.” In it, we dove deep into the importance of healthy fats for metabolic health, and the destructive nature of linoleic acid-rich vegetable oils.
Linoleic acid (LA) is one of the most perishable molecules in food, meaning it’s highly susceptible to damage. When it oxidizes, it turns into oxidative metabolites called oxidative linoleic acid metabolites or oxylipids or OXLAMs that damage proteins, DNA and cell membranes and are likely the primary culprit of chronic disease.
OXLAMs also activate pathways that destroy your immune response. What we didn’t fully appreciate at the time was that even healthy oils, such as olive oil, can have a negative impact, thanks to their LA content. LA is also high in conventionally raised chicken, as these animals are typically fed LA-rich grains.
If you exceed 10 grams of LA per day, and perhaps as little as 5 grams — regardless of their source — you may radically worsen your metabolic health. From a historical perspective, 150 years ago, the average consumption of LA was 2 to 3 grams. Today, many get more than 30 grams a day from their diet. In my view, an LA-restricted diet may be the single most important dietary intervention available.
DiNicolantonio adds:
“That’s a great point, and I think from a COVID-19 perspective, the biggest thing you want to do is increase the resilience of your cells to oxidative stress. Unfortunately, if you’re consuming a diet high in LA, and if it doesn’t get burned for fuel and it gets stored in tissues, the half-life of LA is 680 days, and it can start oxidizing the cellular membranes, including on your immune cells as well.
If you increase your omega-6 intake, that affects the levels in your immune cells. And if you saturate your immune cells with this oxidized LA, you’re probably at a much higher risk of secreting more proinflammatory cytokines in your own cells, and your lungs and your arteries are probably much more susceptible to the damage that occurs when our body tries to kill off viruses.
I’m sure if we were to actually look at the blood levels of oxidized LA in severe COVID-19 patients, they would be sky high … So yeah, it’s likely a huge driver of overall inflammation.”
Simple Strategies to Improve Your NAD+ Level
Another important molecule is nicotinamide adenine dinucleotide (NAD+), which can be increased using precursors such as nicotinamide mononucleotide (NMN) and/or nicotinamide riboside (NR).
NMN appears to be the superior of the two, as it activates a salvage pathway. However, you don’t need to take an expensive supplement to improve your NAD+ level. Strategies such as exercise, hot or cold exposure and time-restricted eating — which costs you nothing — can get the job done. Land explains:
“A lot of the NAD that your body produces is recycled through the salvage pathway. Very little (less than 1%) of it is going to come from food, especially tryptophan or niacin.
The easiest way to prevent losing your NAD as you get older or as you get immunocompromised is to promote the salvage pathway, and one of the activators of this NAMPT enzyme that governs the salvage pathway is AMP protein kinase (AMPK), and AMPK gets primarily turned on by catabolic stressors in the body, such as exercise, sauna, cold, as well as fasting.
What I’ve concluded is that doing this regular intermittent fasting or timed eating is a very efficient way of keeping our energy levels high and preventing the lowering of the other things that lower NAD, like inflammation and oxidative stress.
The problem is that NAMPT is controlled by sirtuins and sirt1 especially. Sirtuins are longevity genes. Sirtuins also control your circadian rhythms. So, what I think is that if your circadian rhythms are misaligned, if you’re doing shift work or you’re jet lagged or something, then sirtuins are not going to be expressed, and you will also then inhibit NAMPT, which will then shut down the NAD salvage pathway.”
In other words, when sirtuins are suppressed from mismatched circadian rhythms, you also suppress NAMPT, as the NAMPT requires sirtuins to work. Sirtuins also consume NAD, so if your NAD level is low, you’re not going to get the benefits sirtuins provide.
“I think the supplemental NR and NMN are very useful if you’re in an NAD-deficient state because the problem is that if you’re already low in NAD, then it’s hard to raise that bar because you’re already so low and depleted,” Land says.
“If your NAD is high, then you experience the less negative side effects from inflammation oxidative stress because your body can repair and deal with it, whereas if you’re immunocompromised, you’re very old or you are just nutrient deficient and have low NAD, then it’s a vicious feedback loop. So, using something like a NAD precursor or a booster can be a quick fix to get yourself back on the right track.”
If you use an NAD or NMN supplement, consider getting it in suppository form. Other alternatives include subcutaneous or intranasal administration, all of which are more effective than oral supplements. That said, as noted by DiNicolantonio, if your NAD is low, your best bet is to address the underlying cause rather than simply adding supplements.
“Ultimately, any type of oxidative stress is going to deplete NAD. So, fix your metabolic dysfunction and improve your nutrient deficiencies first, and ultimately your NAD need is going to go down. Fix the things that are causing you to burn through your NAD.”
One of the most common sources of oxidative stress is electromagnetic field (EMF) exposure, which is the topic of my book “EMF*D.” Two primary enzymes consume NAD. One is poly ADP-ribose polymerases (PARP), which is also known as adenosine ribosyl transferase (ARTD). PARP is used to repair DNA damage, and every time PARP is activated, it uses up 150 molecules of NAD.
The good news is that strategies such as sauna, exercise and fasting not only will improve the production of NAD, but also will reduce the consumption of it. These strategies also lower inflammation, which in and of itself will lower your NAD consumption.
Other Benefits of Sauna Bathing
In addition to preserving your NAD, sauna bathing also mimics a fever, which is your body’s first-line defense against infections. DiNicolantonio explains:
“The reason why we induce a fever to fight an infection is because that allows our cells to secrete heat shock proteins. In order for a virus to replicate, it has to infect your cell, hijack your machinery, and it has to export its ribonucleoprotein complex out of the cell to replicate. In order for that complex to get exported, the M1 protein has to dock onto it.
Heat shock protein 70, which gets released during sauna sessions, can combine to the viral ribonucleoprotein complex preventing M1 protein from docking. [By] inhibiting the export of that viral ribonucleoprotein complex, [heat shock protein] essentially inhibits viral replication.”
According to Land, regular sauna bathing and exercise are among the best things you can do to strengthen your immune system and increase your body’s resilience. The two are also complementary.
Exercise causes preconditioning hormesis, so if you exercise before your sauna, then you significantly bolster your body’s ability to handle infection and other stresses. The heat will also promote recovery from the exercise by boosting growth hormone, repairing damaged proteins and reducing inflammation.
More Information
This interview merely touches on a small number of highlights of the information found in “The Immunity Fix,” so to learn more, be sure to pick up a copy. To connect with DiNicolantonio and Land, see their websites, DrJamesDinic.com and SiimLand.com. Both can also be found on Twitter and Instagram by searching for DrJamesDinic (@drjamesdinic) and Siim Land.
[ad_2]
Source link